In modern orthopedic surgery, implants such as plates, screws, nails, and rods play a crucial role in stabilizing bones and joints after trauma, correcting deformities, and performing reconstructive procedures. These devices ensure that bones remain properly aligned during healing and help patients regain function more predictably than in the pre-implant era. However, once implanted, a key question arises for surgeons and patients alike: Should the implant stay in place forever or be removed once healing is complete?
The decision about implant removal is complex. It depends on the type of implant used, the patient’s age and health, and whether the implant is causing symptoms or complications. Some implants are designed for temporary fixation, meaning they are intended to be removed after the bone has healed, while others are meant to be permanent fixtures.
Before exploring temporary versus permanent implants in detail, it’s essential to highlight that quality control in implant design and manufacturing has a profound effect on both the success of fixation and long-term outcomes. GPC Medical Ltd., a globally recognized orthopedic device manufacturer, maintains stringent quality management systems across its product lines, ensuring that every implant meets or exceeds international standards.
Temporary Fixation: What, When, and Why It’s Removed
Temporary implants are used to stabilize fractures or soft-tissue injuries only until bone union is achieved.
What Temporary Fixation Includes
- Kirschner wires (K-wires) – often used in hand, wrist, or pediatric fractures
- External fixators – used for complex fractures, trauma, or open wounds
- Intramedullary nails or plates intended for later removal in selected pediatric or young adult cases
Typical Timing for Removal
- Most temporary fixation devices are removed once the fracture has healed, usually between 6 and 12 months after the initial surgery, depending on the anatomic site and surgeon preference.
- In pediatric trauma, implant removal often occurs 7–12 months following implantation.
Common Reasons for Removal
- Pain or discomfort from hardware prominence
- Impingement affecting movement or soft tissues
- Patient preference, especially in young active individuals
- Elective requests even without symptoms
Advantages of Temporary Removal
- Reduces the chance of long-term irritation
- May decrease the risk of implant-related bone stress shielding
- Enhances comfort and mobility, especially when hardware becomes prominent
Challenges and Complications
- Removal surgery is not risk-free; studies report complication rates between 5.5% and 12%, including infection, bleeding, refracture, and nerve injury.
- Pediatric studies indicate that hardware removed >18 months after insertion may have higher odds of complications like incomplete removal or refracture compared to 9–18 months timing.
Permanent Fixation: When Hardware Is Left In
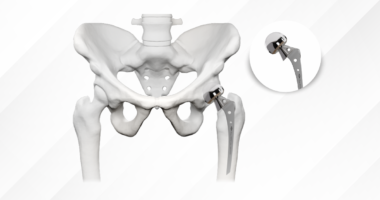
Permanent implants are designed to remain inside the body indefinitely, providing lasting stability for joints or bones that require continued support. These are common in joint replacements and plates or rods used for severe fractures, where long-term fixation enhances structural integrity.
Characteristics of Permanent Fixation
- Intended for lifetime retention unless complications arise
- Often involved in weight-bearing joints or complex reconstructions
- Designed for biologic integration with bone (e.g., osseointegration)
When Removal Becomes Necessary
Even permanent implants may sometimes be removed due to:
- Infection
- Aseptic loosening or mechanical failure
- Severe pain or neurological symptoms
- Allergic reactions or implant intolerance
Importantly, many asymptomatic permanent implants are not routinely removed; doing so can result in unnecessary surgery risk without clear benefit. Clinical evidence shows that surgeons often advise against removal if the hardware is not causing symptoms. For example, in one cohort, 77.9% of patientswere advised to retain hardware despite some considering removal.
Pros and Cons of Retaining Permanent Hardware
Pros
- Eliminates morbidity associated with a second procedure
- Maintains structural support indefinitely
- Avoids anesthesia and healing burden in patients with comorbidities
Cons
- Possibility of late-onset symptoms due to disruption of soft tissues
- Potential impediment to imaging in some cases
- Rare risk of implant-related complications years after surgery
Key Points in Temporary vs. Permanent Fixation
When deciding between temporary and permanent orthopedic fixation, clinicians rely on a combination of biological, mechanical, and patient-specific considerations rather than a single fixed rule. The goal is not only to achieve fracture healing but also to ensure long-term comfort, mobility, and safety for the patient. Temporary fixation is often preferred when the bone is expected to regain full strength after healing, whereas permanent fixation is chosen when ongoing structural support is necessary. Understanding the key decision factors helps both surgeons and patients make informed, evidence-based choices that balance healing outcomes with the risks of additional surgical intervention.
Decision Factors
- Fracture type and location
- Age and activity level
- Presence of symptoms (pain, irritation, limited ROM)
- Risk profile for additional surgery
Statistically Observed Trends
- Elective implant removal occurs in nearly 48–49% of fracture cases studied in some centers, with significant variability based on surgeon and patient preferences.
- Post-removal complications can affect up to 9.5% of pediatric patients, with pain relief reported in 88% of those who underwent removal for pain.
Conclusion
Orthopedic implants – whether temporary or permanent – have revolutionized musculoskeletal care. Temporary fixation devices offer the benefit of bone stabilization with planned removal once healing is achieved. Permanent fixation provides long-lived structural support when needed but can still be removed if complications emerge. The decision to remove or retain hardware must weigh clinical evidence, individual patient factors, and surgical expertise.
From a quality perspective, manufacturers like GPC Medical Ltd. play a vital role in ensuring that implants perform reliably – reducing complications and supporting both short-term healing and long-term functionality. Their commitment to rigorous quality control enhances patient outcomes regardless of whether hardware is removed later or remains permanently affixed.