A fracture is never just a break in bone. It is a disruption of anatomy, biomechanics, mobility, and often, livelihood. Whether caused by a high-velocity road traffic accident, a workplace injury, or a simple fall in the elderly, fractures demand more than immobilization. They require precision, stability, and biological respect. This is where trauma implants play a decisive role, quietly transforming chaos into controlled healing.
Modern orthopedic trauma care is built around one core principle: restore alignment, provide stability, and allow biology to do the rest. Trauma implants are the tools that make this possible.
Understanding Bone Healing: Why Fixation Matters
Bone healing is a complex physiological process, not a passive event. It unfolds in phases—inflammation, repair, and remodelling – each sensitive to movement, blood supply, and mechanical stress. When fragments move excessively or alignment is compromised, healing falters. Non-union, malunion, and chronic pain follow.
Trauma implants are designed to control this micro-environment.
By holding fractured segments in optimal alignment, implants convert uncontrolled motion into constructive strain, stimulating callus formation rather than disrupting it. The result is predictable healing, reduced pain, and earlier return to function.
What Are Trauma Implants?
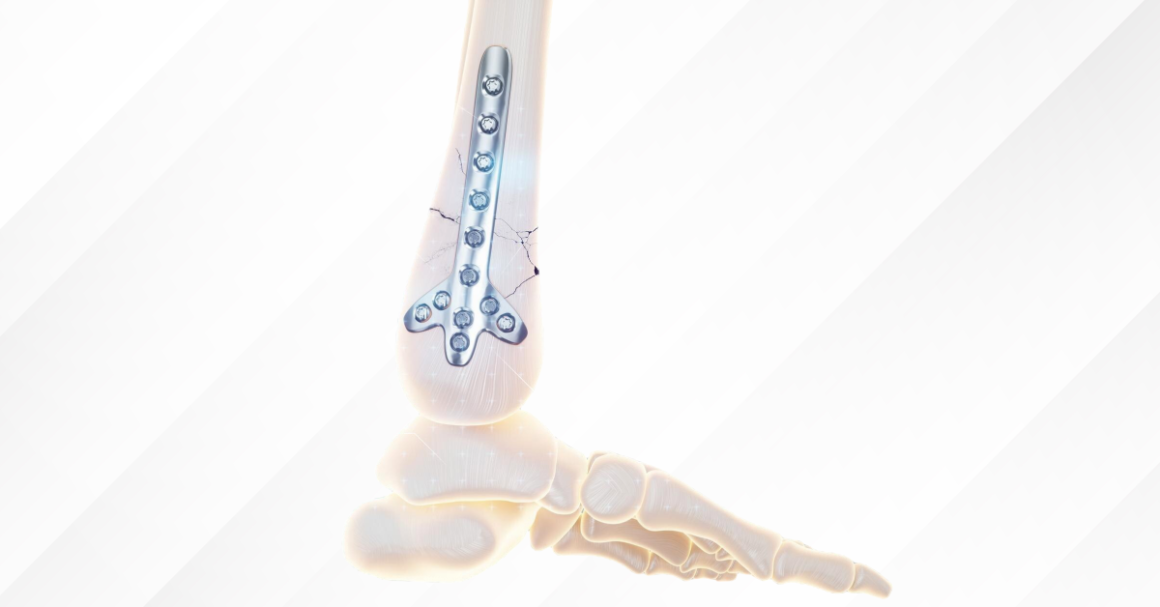
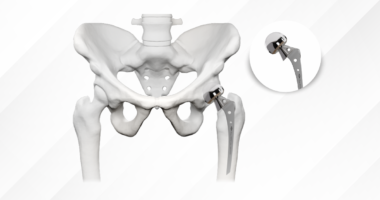
Trauma implants are medical devices used to stabilise fractured bones internally or externally until healing occurs. Unlike casts or braces, implants work beneath the skin, providing rigid or semi-rigid support directly at the fracture site. They are engineered to withstand load, resist fatigue, and interact safely with bone tissue over weeks or months – sometimes permanently.
How Trauma Implants Support the Healing Process
Trauma implants do not “heal” bones. They create the conditions in which healing becomes inevitable.
One concise way to understand their role is through the mechanical and biological advantages they provide:
- Maintain anatomical alignment
- Control micro-motion at the fracture site
- Protect surrounding soft tissues
- Preserve blood supply to bone
- Enable early mobilisation and rehabilitation
This balance – between stability and biological respect – is what defines modern fracture care.
Quality That Defines Outcomes: Why Trauma Implant Standards Matter
Trauma implants are subjected to continuous biomechanical stress, repetitive loading, and complex physiological environments. Even minor deviations in material composition, surface finish, or dimensional accuracy can translate into implant failure, delayed union, or catastrophic loss of fixation. Quality, therefore, is not merely about compliance; it is about predictability, safety, and long-term performance inside the human body.
GPC Medical Ltd. treats quality as an essential clinical requirement, not merely a manufacturing formality. The company has instituted multi-layered quality control mechanisms that span the entire production lifecycle. These include stringent incoming material inspections, in-process dimensional verification, surface integrity assessments, and final product validation aligned with international standards.
The company ensures high-quality implants, showcasing consistent load-bearing capacity, corrosion resistance, and biocompatibility – factors that reduce complications, revision surgeries, and post-operative morbidity.
By embedding quality control into both design philosophy and manufacturing execution, GPC Medical Ltd. delivers trauma implants that surgeons can rely on and patients can heal with – consistently, safely, and predictably. In trauma fixation, where margins for error are minimal, such uncompromising quality standards are not just important; they are essential.
Trauma Implants and Early Mobilization
One of the most significant advantages of modern fixation is early functional recovery. Prolonged immobilization carries risks – joint stiffness, muscle atrophy, thromboembolism, and pulmonary complications.
Stable fixation allows:
- Early joint movement
- Partial or full weight-bearing where appropriate
- Reduced hospital stay
- Faster return to daily activities
In elderly patients, this can be the difference between independence and long-term disability.
Special Considerations in Complex Trauma
Complex trauma scenarios demand a more nuanced approach to fracture fixation, where implant selection and surgical strategy must account not only for the fracture pattern but also for biological vulnerability, soft-tissue condition, and long-term functional implications. In cases such as open fractures, osteoporotic injuries, and pediatric trauma, standard fixation principles often require modification. The goal shifts from achieving immediate rigidity to balancing stability with tissue preservation, infection control, and future growth or bone quality considerations. It is within these challenging contexts that thoughtful implant choice and staged decision-making become critical to successful outcomes.
Open Fractures
Open fractures present a dual challenge – bone injury and contamination.
- External fixation often used initially
- Definitive internal fixation delayed until infection risk is controlled
- Implant choice must prioritise soft-tissue healing
Osteoporotic Fractures
Poor bone quality compromises screw purchase.
- Locking plates improve fixation strength
- Cement augmentation may be used
- Implant positioning becomes critical
Paediatric Fractures
Children are not small adults.
- Flexible nails preferred in many long-bone fractures
- Growth plates must be protected
- Implant removal is more commonly planned
Implant Removal: Is It Always Necessary?
Not all trauma implants need to be removed. The decision depends on symptoms, location, patient age, and implant type.
- Symptomatic implants causing pain or irritation may be removed
- Implants in children are more often removed
- Deep, asymptomatic implants are often left in place
Routine removal without indication is no longer standard practice.
Conclusion: Engineering Stability, Enabling Biology
From fracture to fixation, trauma implants serve as silent partners in recovery. They do not replace the body’s healing capacity; they organise it. By restoring alignment, controlling motion, and respecting biology, these devices convert traumatic disruption into structured repair.
In modern orthopaedics, successful fracture management is no longer measured solely by radiographic union, but by how quickly and safely a patient returns to function. Trauma implants make that journey possible – precisely engineered, biologically informed, and clinically indispensable.