Implant success does not begin in the operating theatre. It begins much earlier, at the level of material science. Long before fixation techniques, surgical precision, or rehabilitation protocols come into play, one decision quietly determines outcomes: the choice of implant material.
Biocompatibility is not a buzzword. It is a biological negotiation between metal and living tissue – sometimes harmonious, sometimes hostile. Among the most commonly used materials, titanium and stainless steel dominate orthopedic, dental, and trauma implants. Both have strengths. Both have limitations. And the difference between long-term success and silent failure often lies in how well these materials coexist with the human body.
Understanding Biocompatibility in Implant Design
Biocompatibility refers to a material’s ability to perform its intended function without eliciting undesirable local or systemic responses. In implants, this translates into a delicate balance – mechanical strength must coexist with biological tolerance.
From the body’s perspective, any implant is a foreign object. The immune system evaluates it. Surrounding tissues respond. Cells either integrate or isolate. The outcome of this interaction determines whether an implant becomes part of the body – or remains an intruder.
Key factors influencing biocompatibility include:
- Chemical composition of the material
- Surface texture and oxide layer stability
- Resistance to corrosion and wear
- Interaction with bone, soft tissue, and blood
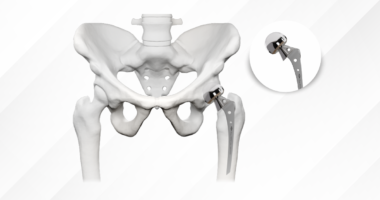
Why Material Selection Directly Impacts Implant Longevity?
Implant failure is rarely dramatic. It is often gradual. Subtle. Missed in early imaging. A poorly chosen material may initially function well, only to trigger inflammatory reactions, bone resorption, or mechanical loosening years later.
Material selection affects not only biological response but also mechanical harmony. An implant that is too stiff can shield bone from physiological stress, leading to bone loss. Longevity, therefore, is not merely about strength – it is about compatibility over decades, under repetitive loading, within a chemically active biological environment.
Material choice influences implant success by affecting:
- Osseointegration and bone remodeling
- Stress distribution at the bone – implant interface
- Risk of corrosion and metal ion release
- Long-term mechanical stability
Titanium Implants: The Benchmark of Biocompatibility
Titanium defining advantage lies in the formation of a stable, inert titanium oxide layer when exposed to oxygen. This layer acts as a biological shield, preventing corrosion and minimizing immune reactions.
More importantly, titanium actively supports osseointegration. Bone cells adhere to its surface, grow along it, and anchor the implant in place. This is not passive tolerance—it is biological cooperation.
Despite being lighter than stainless steel, titanium exhibits an excellent strength-to-weight ratio, making it ideal for long-term implants where fatigue resistance is critical.
Clinical advantages of titanium implants include:
- Superior osseointegration and bone bonding
- Excellent corrosion resistance in physiological environments
- Reduced inflammatory and allergic reactions
- Lower modulus of elasticity, closer to that of bone
Stainless Steel Implants: Strength with Biological Trade-offs
Stainless steel, particularly 316L surgical grade, has long been used in orthopedic and trauma applications. It offers high tensile strength, ease of manufacturing, and cost-effectiveness. For temporary implants, it often performs adequately.
However, stainless steel is not biologically inert. It contains nickel and chromium—elements known to provoke hypersensitivity reactions in susceptible individuals.
Common characteristics of stainless steel implants:
- High initial mechanical strength
- Greater stiffness than cortical bone
- Potential for corrosion and ion release over time
- Higher risk of allergic or inflammatory responses
Titanium vs Stainless Steel: A Comparative Clinical Perspective
Titanium tends to integrate. Stainless steel tends to coexist—sometimes uneasily. In load-bearing, long-term applications such as joint replacements or dental implants, titanium consistently demonstrates superior outcomes.
Stainless steel, by contrast, remains useful in temporary fixation devices, fracture plates, and cost-sensitive scenarios where long-term integration is not essential.
Key differences influencing implant success:
- Titanium promotes bone growth; stainless steel does not
- Stainless steel is stiffer, increasing stress-shielding risk
- Titanium has lower corrosion potential
- Stainless steel carries higher hypersensitivity risk
From Material Selection to Implant Performance: GPC Medical’s Manufacturing Framework
At GPC Medical, titanium and stainless steel are not treated as interchangeable metals; they are deployed where their biological and functional strengths are most relevant. This clarity underpins GPC Medical’s manufacturing framework, ensuring that implant performance is driven as much by biocompatibility as by mechanical precision.
For critical orthopedic and trauma implants, GPC Medical prioritizes titanium and its alloys, recognizing their superior interaction with bone and soft tissue. From raw material procurement to final surface finishing, titanium components are processed under tightly controlled parameters to preserve structural integrity and biological compatibility.
Titanium implant manufacturing at GPC Medical focuses on:
- High-purity titanium alloys suitable for long-term implantation
- Precision CNC machining and controlled finishing for surface consistency
- Design optimisation to support osseointegration and load distribution
- Rigorous mechanical and corrosion resistance testing
- Titanium implant portfolio, which includes titanium rods, the Titanium Elastic intraHEAL Nailing System, and advanced intramedullary devices such as the intraHEAL Proximal Hip Stabilizing Nail.
GPC Medical manufactures a wide range of stainless steel dressing drums, sterilisation boxes, holloware, and hospital utility products, all designed to withstand repeated autoclaving and intensive clinical use. In laboratory equipment, medical diagnostic accessories, and hospital furniture components, stainless steel provides structural reliability without direct interaction with living tissues, making its biological limitations clinically irrelevant in these contexts.
Stainless steel applications within GPC Medical’s general medical division include:
- Hospital holloware and utility products
- Dressing drums and sterilization containers
- Laboratory and diagnostic equipment components
- Reusable medical accessories requiring high structural stability
Future Directions in Biocompatible Implant Materials
Material science continues to evolve. Titanium alloys with improved fatigue resistance, nickel-free stainless steels, and bioactive coatings are pushing boundaries. Additive manufacturing now allows patient-specific implant design, optimizing both mechanical and biological compatibility.
Yet, the core principle remains unchanged: biocompatibility is foundational, not optional. No amount of surgical skill can compensate for a material that the body ultimately rejects.